Insulin Medications: A Comprehensive Guide
The pancreas secretes the hormone insulin, which is the key player in the complex system that keeps the body's blood sugar levels under control. Its importance cannot be overstated, especially for those suffering from diabetes, whose bodies are less able to make or use insulin as intended. Appropriate insulin control is essential for health; it goes beyond simple dosing and timing. Given the wide range of insulin drugs available, it is essential to understand the subtle differences between them to successfully change treatment programs to each patient's specific needs.
What is Insulin
Insulin, a peptide hormone secreted by the pancreas, serves as a crucial regulator of blood glucose levels in the body. Upon food consumption, especially carbohydrates, insulin is released into the bloodstream, signaling cells to absorb glucose for energy production or storage. It plays a pivotal role in maintaining stable blood sugar levels, ensuring cells receive the necessary energy for optimal function.
Relationship Between Insulin Production And Diabetes
One essential hormone that the pancreas produces is insulin, which plays a critical role in controlling the body’s levels of glucose, or blood sugar. The body starts breaking down food, especially carbs, into glucose when it is consumed. This glucose then enters the bloodstream. Insulin functions as a molecular key that makes it easier for cells throughout the body to absorb glucose so they may either use it immediately for energy generation or store it for later.
This process is necessary to keep blood glucose levels steady and guarantee that cells get the energy they require to perform at their best.
Diabetes Types
Diabetes is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia). There are primarily two types of diabetes:
- Type 1 Diabetes: This results from the immune system attacking and destroying insulin-producing beta cells in the pancreas. As a result, the pancreas produces little to no insulin. People with type 1 diabetes require insulin injections for survival.
- Type 2 Diabetes: This develops when the body becomes resistant to the effects of insulin or doesn’t produce enough insulin to maintain normal blood sugar levels. Initially, the pancreas may compensate by producing more insulin, but over time, it may not keep up with demand.
Insulin Production and Type 1 Diabetes
When a person has type 1 diabetes, their immune system mistakenly attacks the beta cells in the pancreas that produce insulin. The autoimmune attack causes these essential cells to gradually degrade, which in turn causes the synthesis of insulin to decrease or stop entirely. Reduced insulin levels obstruct cells’ ability to absorb glucose, leading to a build-up of glucose in the blood. If left untreated, persistently high blood sugar levels can lead to a wide range of issues. These consequences can include a wide range of medical conditions, from kidney malfunction and nerve damage to cardiovascular difficulties.
Insulin Production and Type 2 Diabetes
One of the main causes of type 2 diabetes is insulin resistance, a disease in which cells all over the body show decreased sensitivity to the actions of insulin, which prevents the body from absorbing glucose. The pancreas initially increases insulin production as a compensatory mechanism to overcome resistance and keep blood sugar levels within a healthy range.
However the pancreas may eventually get overworked due to this increased secretion of insulin, and its capacity to maintain such high levels of production may gradually diminish. As a result, insulin secretion may decrease, worsening the blood glucose build-up. Furthermore, poor food choices, physical inactivity, and obesity are lifestyle variables that might worsen insulin resistance and further impede insulin production, which will accelerate the onset of type 2 diabetes.
Here’s a detailed overview of some common insulin medications:
Rapid-Acting Insulins:
- Admelog SoloStar (Insulin Lispro)
- Apidra (Insulin Glulisine)
- Fiasp (Insulin Aspart)
- Humalog (Insulin Lispro)
- Novolog (Insulin Aspart)
Short-Acting Insulins:
- Humulin R (Human Biosynthetic Insulin Injection)
- Novolin GE Toronto (Human Biosynthetic Insulin Injection)
Intermediate-Acting Insulins:
Long-Acting Insulins:
- Basaglar (Insulin Glargine)
- Lantus (Insulin Glargine)
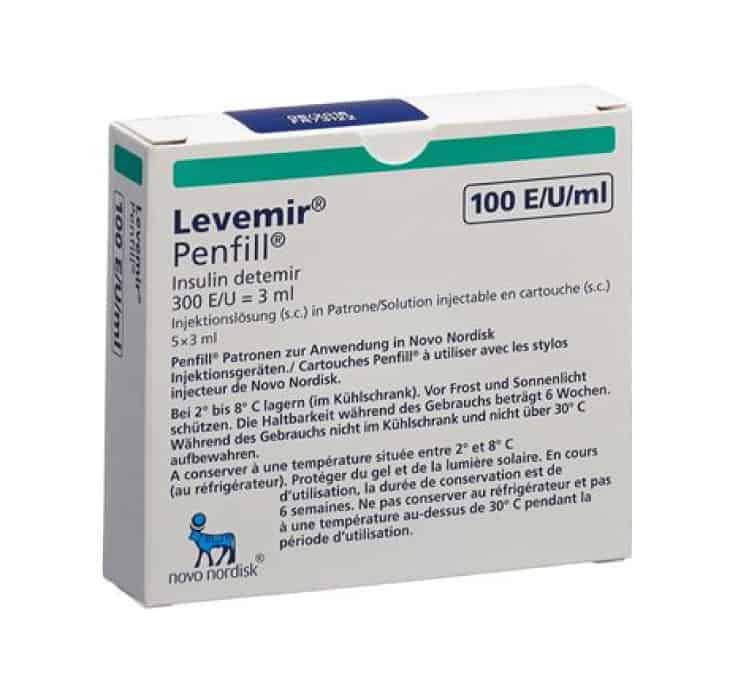
- Levemir (Insulin Detemir)
- Toujeo (Insulin Glargine)
- Tresiba (Insulin Degludec)
Mixed Insulins:
- Humalog Mix (Insulin Lispro)
- NovoMix (Insulin Aspart)
- Novolin GE Mix (Insulin Isophane)
Combination Insulins:
- Soliqua (Insulin Glargine and Lixisenatide)
- Xultophy (Insulin Degludec and Liraglutide)
- Entuzity (Insulin Human and Insulin)
When choosing an insulin medication, factors such as the onset of action, duration, and flexibility of the dosing schedule should be considered. It’s crucial to work closely with a healthcare provider to determine the most appropriate insulin regimen for individual needs.
Apidra
Basaglar
Fiasp
Humalog
Humulin
Lantus
Levemir
Novolin
NovoRapid (Novolog)
Tresiba
Other Insulin Brands
Frequently Asked Questions
Insulin is a natural hormone responsible for regulating blood sugar and many other processes in the human body. It’s produced by beta cells in the pancreas during digestion and helps body cells absorb glucose and turn it into energy. People with Diabetes either cannot produce insulin (Type 1) or don’t process it effectively (Type 2). For this reason, they need to take insulin in order to metabolize glucose.
Insulin works by moving glucose from your bloodstream into your body’s cells. It’s the agent that makes it possible for your cells to receive blood sugar (glucose) and turn it into energy for your body. Without insulin, glucose can’t enter your cells and builds up in your blood instead. This results in hyperglycemia (high blood sugar), which is one of the major concerns for people with Diabetes.
People take different types of insulin based on how quickly they need it to start acting and reach its peak (maximum) impact. Other factors include how long it lasts, how concentrated it is, and the method of delivery (subcutaneous injection, intravenous injection, or inhalation). Some common insulin types are:
- Rapid-Acting Insulin (begins working within 5-20 minutes and peaks 1-2 hours after injection)
- Regular/Short-Acting Insulin (begins working within 30 minutes and is effective for 3-6 hours)
- Intermediate-Acting Insulin (begins working within 2-4 hours and peaks after 4-12 hours later)
- Long-Acting Insulin (begins working several hours after injection and is effective for up to 24 hours)
- Ultra Long-Acting Insulin (begins working within 6 hours and lasts 36 hours or longer)
Patients with Type 1 Diabetes always require insulin. People with Type 2 Diabetes and other types of Diabetes may or may not require insulin on a regular basis. In certain circumstances, insulin may also be prescribed for patients suffering from other conditions (see Question 10 below).